HubStar for Healthcare
Top Two NHS Trust Space Optimization Challenges in 2025
On June 11th, we were joined by three senior estates and property leaders - Lee Whitbread from South West London ICB, Phil Boorman from Sussex Partnership NHS Trust, and David Mander from Royal Berkshire NHS Trust for an insightful discussion on the best ways to manage and allocate both corporate and clinical spaces. Here are our top two takeaways from the virtual panel.

The NHS estate is worth £12 billion and growing. But underneath that growth, a challenge is lurking: how to make existing space work harder without the budget for major investments.
In our recent virtual panel, we were joined by three senior estates and property leaders – Lee Whitbread from South West London ICB, Phil Boorman from Sussex Partnership NHS Trust, and David Mander from Royal Berkshire NHS Trust for an insightful discussion on the best ways to manage and allocate both corporate and clinical spaces.
Here are our top two takeaways from the panel, plus four steps to optimize NHS spaces moving forward.
Watch the whole virtual panel right here!
Watch the recording to get the full scoop on how our panelists are dealing with these space optimization challenges within their own organizations.
Takeaway #1: Space planning for corporate vs clinical spaces is a very different beast.
Unlike traditional office environments, NHS trusts face a unique complexity: the difference between clinical and corporate space and workforce requirements.
Corporate spaces are the easier win, since teams have adapted relatively well to hybrid working. As Lee Whitbread from NHS South West London ICB explained: “We cut our space in half, from two floors to one, and learned to adapt quite quickly.”
This downsizing was made easier by:
- Directorate rotation schedules (teams come in once per fortnight)
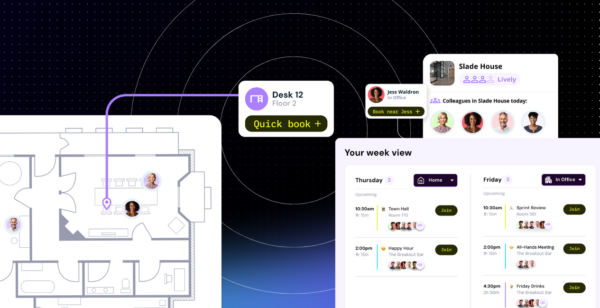
- Desk booking systems with 150 desks for 450 employees
- Flexible drop-in spaces and collaboration areas
Clinical spaces, on the other hand, present a different challenge entirely. Phil Boorman from NHS South West London ICB described the typical clinical day: “You come in, use a desk for emails, attend a team meeting, go to a clinical room for patient appointments, maybe do a home visit, then return to write up notes.”
This variability makes traditional space planning models inadequate. Clinical teams need:
- Immediate access to specialized equipment
- Confidential spaces for patient discussions
- Flexible scheduling around patient care
- Team collaboration spaces for handovers
One-size-fits-all approaches don’t work. Clinical spaces require different utilization targets and measurement approaches than corporate areas.
Takeaway #2: Technology fragmentation is prevalent and comes at a cost.
The second major challenge emerged around technology fragmentation, which is costing trusts both money and efficiency.
As Phil Boorman highlighted: “We’re very good at reinventing the wheel in the NHS. We’ll have one system for booking, another for workplace management, another for sensors, but none of these systems talk to each other.”
This fragmentation creates several problems:
- Siloed data: No unified view of space utilization
- Inefficient resource sharing: Trusts can’t share underutilized spaces with neighboring organizations
- Higher costs: No savings from bundled solutions or platforms
The solution isn’t just better individual tools, it’s integrated systems that work together:
- Motion sensors for detailed utilization data
- Access control data for attendance patterns
- WiFi analytics for broader occupancy insights
- Booking systems that connect across trust boundaries
4 Space Optimization Tips for NHS Trusts
Over the course of the discussion, four ways to improve space planning, management and allocation came up.
1. Start with data.
“Get some data. It doesn’t matter what it is, but just get some tangible data,” advised Phil Boorman. Whether it’s:
- Booking system analytics
- Access control data
- WiFi connection counts
- Motion sensors (where budget allows)
2. Set clear standards and stick to them.
A set of guidelines, transparency around them, and data to back it up (ideally) makes space allocation conversations with employees much smoother. It’s only natural to feel miffed when the desk or space you’re used to having 100% of the time doesn’t fully belong to you anymore, so clearly articulated standards go a long way here.
David Mander’s approach: “We have a very clear path and robust standards. If the answer is no, we come back to the standards to work out why.”
3. Design both corporate and clinical spaces for activity-based working.
Create spaces for different types of work:
- Confidential meeting pods for sensitive discussions
- Collaboration areas for team meetings
- Quiet zones for focused work
- Drop-in spaces for flexibility
4. Get executive buy-in early
“Execs are often the people that undermine hybrid working the most because they want to people-please,” noted David Mander. So it smoothes over the entire process to secure leadership commitment before implementing changes and starting the change management process.
The NHS can’t afford to treat space as an unlimited resource anymore. With trusts like Royal Berkshire operating on “island sites” with no room to expand, and others facing 15-year delays on promised new hospitals, it’s critical to get more from existing spaces.
The trusts leading this transformation are saving money and improving patient outcomes. As David Mander observed: “Sitting next to the person you’re going to email improves patient flow, patient output, and patient health.”
The question isn’t whether your trust needs better space utilization, it’s whether you’ll lead the change or be forced into it by financial pressures.
Watch the whole virtual panel right here!
Watch the recording to get the full scoop on how our panelists are dealing with these space optimization challenges within their own organizations.
Share this post